Vaccine sovereignty and international law
Can international norms prioritise humanity before sovereignty? A pertinent question in the context of current vaccine hoarding.
My country first
As the pandemic shook the planet, governments immediately switched to a defensive ’my population first’ mode. This was apparent from closed borders, masks being seized, exports being banned and the hoarding of vaccines. Narrow sighted as it seems now, it was a reflection of the classical raison d’Etat – the need for society to govern and protect itself. After all, the principles of non-interference (implying jurisdiction over people and territory) and equality (implying territorial integrity, non-intervention, diplomatic immunity, legal personality of States) remain core values of today’s international system, enshrined in the UN Charter. Sovereignty also implies the obligation to implement the norms of international law in force, as a corollary of the right to conclude treaties. But in the context of today’s vaccine hoarding, can international norms prioritise humanity before sovereignty?
Sovereignty determines the allocation of ownership and control of vaccines (and other pharmaceuticals): the country in which vaccines and drugs are manufactured has unquestionable sovereignty over such resources until they leave its territory, and the country to which vaccines and drugs are imported or sold then has sovereignty over them under international law. Thus, any strategy to increase access to vaccines and drugs through a global framework faces a ‘triple sovereignty problem’: it must address claims of sovereignty where the virus strains are isolated; where vaccines or drugs are manufactured; and finally where vaccines and drugs are sold or exported. Sovereignty also comprises the obligation to protect (without discrimination) the population within the defined territory.
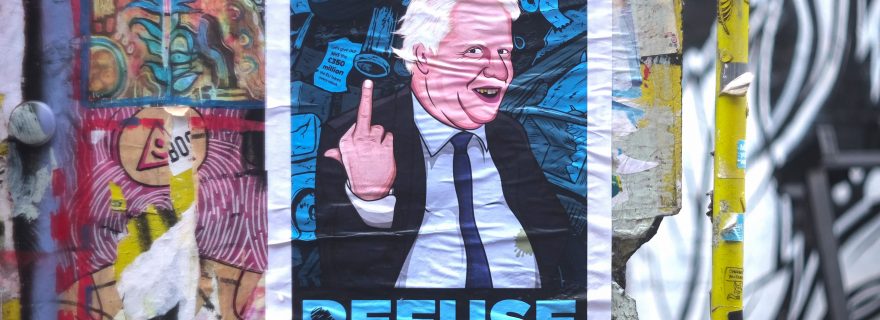
Affordable, non-discriminatory access to the vaccine is a human right. This is clearly stated in the message of the UN OHCHR on 17 December 2020. It underlines the high standard of the obligation of the right to health: everyone is entitled, on an equal footing with others, to enjoy access to all the best available applications of scientific progress necessary to enjoy the highest attainable standard of health. But ‘only after we have completed the national vaccination programme’ corrects Boris Johnson. No-one is claiming the citizens of other countries should be prioritised above your own. Indeed, the obligations related to the right to health in human rights treaties still focus mainly on the States Parties’ responsibilities for their own population. Hence, the right to health has more significance for equitable access within a country’s jurisdiction. However, controversy is destined to escalate as the vaccination rollout advances, revealing further inequalities.
Articles 12 and 15 of the International Covenant on Economic, Social and Cultural Rights and Articles 25 and 27 of the Universal Declaration of Human Rights refer to the right to the enjoyment of the highest attainable standard of physical and mental health and the right to enjoy the benefits of scientific progress. This effectively includes access to a vaccine for COVID-19 that is safe, effective and based on the best scientific developments. States Parties must take steps to achieve the ‘prevention, treatment and control of [the] epidemic’ in accordance with European Social Charter Article 11.(1),(3). According to the Committee on Economic, Social and Cultural Rights (CESCR), established to monitor the implementation of the International Covenant on Economic, Social and Cultural Rights, ‘States therefore have a priority obligation to take all the necessary measures, to the maximum of their available resources, to guarantee access to available vaccines for COVID-19 to all persons, without any discrimination. This obligation needs to be implemented nationally.’ That much is clear, but then it follows: ‘at the same time has also an international dimension as many States worldwide do not produce vaccines themselves. States have therefore a duty of international cooperation and assistance to ensure access to vaccines for COVID-19 wherever needed, including by using their voting rights as members of different international institutions or organizations’ (E/C.12/2021/1). Except, there has always been inequality across the different national health systems including unequal access to health services. Can it be claimed that standards have evolved or is it because the recent pandemic requires this specifically?
International framework
The WHO Constitution contains no legally binding provisions that require WHO member States to increase access to health-related resources for low-income countries except for the preamble’s principle that ‘[t]he extension to all peoples of the benefits of medical, psychological and related knowledge is essential to the fullest attainment of health’. The International Health Regulations of 2005 (IHR 2005) do not include any provisions that directly advance more equitable access to vaccines and drugs. They barely state the obligation ‘to undertake to collaborate with each other, to the extent possible (…) in the provision or facilitation of technical cooperation and logistical support, particularly in the development, strengthening and maintenance of the public health capacities’ (IHR 2005, Art. 44.1(b)). This objective was reaffirmed in the Declaration of Astana (2018) where States reiterated commitments to effective development cooperation and to sharing knowledge and good practices (while fully respecting human rights) in order to prevent, detect and respond to infectious diseases and outbreaks.
The right to health falls short of providing a strong legal foundation on which to build a global access framework. Other existing international legal regimes for global health also fail to formulate imposable rules that could form the basis for the creation of a global access framework. For example, the International Vaccine Institute (IVI) bringing together 36 States Parties to conduct research, training, and technical assistance for vaccines needed in developing countries, does not participate in the debate about equitable access to pandemic vaccines.
Can it be claimed then that the right to equitable access is embedded in political commitments entered into by voting on multilateral documents or by unilateral political declarations highlighting commitments to fight the pandemic globally? The Committee on Economic, Social and Cultural Rights refers in its recent recommendation (E/C.12/2021/1) to the political obligation contained in the Sustainable Development Goals (SDGs): most vaccines have been applied in and reserved for developed and high-income countries, whereas vaccination in many least developed and developing countries has not even started which undermines progress on achieving Sustainable Development Goals, especially SDG 3 on ensuring healthy lives and well-being at all ages, SDG 10 on reducing inequalities within and among countries and SDG 17 on strengthening the means of implementation and revitalising the global partnership for sustainable development. It remains to be seen where the discussion goes in this respect.
More specifically, the humanitarian obligations are addressed in the context of the UN Secretary-General’s global call for solidarity, according to which humanitarian obligations of all States in a position to assist include the following: sharing research, medical equipment, supplies, and best practices; coordinating to reduce the economic and social impacts of the pandemic; limiting economic sanctions, debt obligations, and intellectual property regimes that impede access to needed resources; and, in all this, focus on vulnerable and disadvantaged groups, fragile countries, and conflict and post-conflict situations. Subsequent political commitments provide support for global governance under the UN's COVID-19 Global Humanitarian Response Plan and the UN Framework for the Immediate Socio-Economic Response to COVID-19.
Looking forward
However, despite repeated pleas for global solidarity in the COVID-19 response and in fact, substantial financial contributions, many States in a position to assist have failed so far to provide sufficient international assistance in the form of access to the vaccine resource. This is not the first time vaccine hoarding has been criticised by international organisations. See, for example, the reports by David Fidler on Bird Flu and Swine Flu pandemics where he argues that the self-interested calculations of developed States with respect to supplies of influenza vaccines and antivirals do not create a firm basis for an international agreement on sharing.
Nevertheless, the CESCR argues that States have the international obligation to support, to the maximum of their available resources, efforts to make vaccines available globally. In this regard, it can be claimed that the COVAX Facility was established to ensure all countries will have equal access to any vaccines against the coronavirus disease and countries forming part of it automatically comply with their obligations to support the global action, whatever their national vaccination policies. But perhaps calling for a global access framework by merely appealing to equity, solidarity, and justice is not sufficient? Proponents of greater access often argue that increasing such access to vaccines and drugs represents enlightened self-interest and smart public health. Indeed the Covax Allocation Algorithm contains a logical explication of the advantages of global vaccination. Thus, the international access framework might indeed be considered as part of the duty of the States to protect their populations internally. Many questions remain, however, as to the further responsibility of making sure that access to the vaccines leads to effective vaccination.
To conclude, it is hoped that this mechanism, patched together as the world scrambles to fight a pandemic, becomes the norm for future pandemics. As the Secretary-General put it, global solidarity is not only a moral imperative – it is in everyone’s interest. Prospects to protect all people improve when sovereignty is not viewed as a wall or shield.


0 Comments
Add a comment